Nhan Van Vo DDS, PhD∗Tu Nguyen DDS∗Quan Dong Ta DDS, MS∗Bao Chi Truong DDS
This case report describes an unusual case of implant treatment after contralateral inferior alveolar nerve transposition (IANT) on a unilateral reconstructed mandible due to gunshot trauma with a 7-year follow-up. The patient had an edentulous atrophic mandible and underwent large bone reconstruction on the left side. The irregular passage of the right inferior alveolar nerve was within 1-2 mm of the superior aspect of the mandible, passed through the midline, and was nearly exposed under the oral mucosa at the left anterior part of the mandible, which prevented the placement of conventional implants. Consequently, right IANT followed by iliac onlay bone grafting was undertaken under general anesthesia to create a sufficient bone volume for implant placement. Four implants were installed simultaneously on the augmented bone. After a 2-month waiting period, soft tissue graft placement and vestibuloplasty were performed. The patient was scheduled for a continuous follow-up for the next 7 years. After 3 years, the bar-retained supporting system was replaced with the new CAD/CAM milled bar system on the same 4 implants. The 4 implants presented good initial stability (35 N/cm), and radiographic evaluation showed osseointegration around all 4 implants. The patient experienced lip numbness in the first 5 days postoperatively but recovered by 97% after 2 months. After a 7-year follow-up, the result remained satisfactory with no sign of bone loss around any of the 4 implants, and the prosthesis functioned well and was stable and esthetically satisfactory. In conclusion, an immediate implant placement procedure after a complex surgery involving unilateral IANT and iliac onlay bone grafting remains challenging, especially when the patient has extensive bone defects or an atrophic mandible. However, a successful long-term outcome can be achieved with appropriate perioperative and postoperative care.
One of the most common challenges for implant placement is insufficient bone height and volume.(1) Installing implants without encroaching on the inferior alveolar nerve is nearly impossible, especially in patients with atrophic edentulous posterior mandibles. Several treatment options that do not interfere with the nerve canal have been suggested: vertical ridge augmentation,(1),(2) distraction osteogenesis,(3) guided bone regeneration,(4) and short implants.(5) In more severe cases, another option is nerve transposition.(6)
In 1977, Alling first reported the nerve repositioning technique for the atrophic lower jaw.(7)In 1987, Jensen and Nock (8) utilized the inferior alveolar nerve transposition (IANT) technique for implant placement for the first time. Five years later, Rosenquist (9) performed the first study of IANT on 10 patients using 26 implants, with an implant survival rate of 96%.
One of the disadvantages of IANT is recovering the alveolar ridge. According to Buser et al.,10 these vertical ridge augmentation approaches, especially guided bone regeneration, require multiple surgical interventions, which prolong the postoperative duration and have unpredictable outcomes. In addition, such approaches are not appropriate for patients with advanced posterior bone resorption.(10) To enhance the basal bone in both vertical and horizontal dimensions, an onlay bone graft is recommended. Among some extraoral donor sites, the iliac free bone graft (IBG) has become an optimal choice for bone augmentation to achieve an adequate bone volume.(11)
IANT, combined with onlay bone augmentation and implant placement, is an intricate, technique-sensitive procedure that requires experienced surgeons and strict patient selection. The procedure has a high complication rate, with complications such as lip paresthesia, infection, and mandibular fracture. Thus, this combined approach is not a common operation. However, in cases of advanced alveolar ridge resorption, the combined technique offers some advantages: 1) implants with a suitable length can be placed to achieve biomechanical stability without damaging the inferior alveolar nerve; and 2) the integration of IANT, bone graft and implant placement in 1 procedure reduces the treatment time.
The aim of this case report is to present an unusual case of implant treatment after contralateral IANT and iliac onlay bone grafting on a unilateral reconstructed mandible due to gunshot trauma. This study also illustrates the outcome after 7 years of follow-up, including the survival of the placed implants. In addition, the safety of this technique and complications related to neural function are evaluated.
Case Report
Patient Description
A 59-year-old male patient with a complete edentulous atrophic mandible presented with a chief complaint of a loose-fitting denture that caused pain during function. The left mandible was reconstructed 40 years previously after a gunshot injury by utilizing iliac crest bone. The patient had good medical health and no systemic diseases, such as diabetes or heart disease. He maintained a healthy lifestyle with no history of alcohol or tobacco use. Clinical examinations (orthopantomography and cone-beam computed tomography) showed severe atrophy of the alveolar ridge (class VI, as described by Cawood and Howell (12)) (Fig 1). The crest of the ridge was below the floor of the mouth at the lower level of the genial tubercles with loose connective tissue and no keratinized tissue. Radiographic examination revealed that the inferior alveolar canal was too close to the crest and that the left reconstructed mandibular body deviated out of the mandibular arch. The patient had a bone height of 1-2 mm from the right inferior alveolar canal to the crest of the alveolar ridge, extending from the lower right second molar to the right lower central incisor. The right inferior alveolar nerve passed through the midline and was nearly exposed under the oral mucosa at the anterior part of the mandible (Fig 1). Indeed, the incisive branch of the right inferior alveolar nerve terminated and was exposed at the lower left lateral incisor. The height of the remaining basal bone was also evaluated; particularly, at the position of the lower left canine and the lower left premolar, the height was only 7 mm, which required a bone graft to increase the volume. Moreover, obtuse mandible bone angles are a disadvantage for the placement of implants in a proper direction. As the alveolar ridge was severely resorbed and the inferior alveolar canal was too close to the crest, the guided bone regeneration procedure and conventional implant placement were impossible. Therefore, the surgical plan was right IANT and onlay bone grafting (from the right iliac crest) on the remaining basal bone with immediate placement of 4 implants.
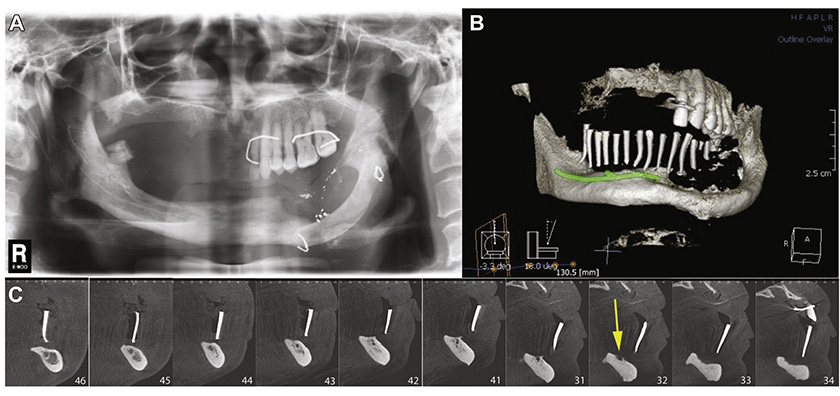
Figure 1. Radiography showed severe atrophy of the alveolar ridge. A, Orthopantomographic view. B, Three-dimensional reconstructed image using multidetector cone-beam computed tomography with illustration of the right inferior alveolar nerve pathway. C, CT slices at positions #46 to #34 showed that the right inferior alveolar nerve was 1-2 mm from the alveolar crest (the arrow shows that the nerve was exposed on the alveolar bone of the left anterior region).
Because this is a case report, institutional review board approval was not required. The requirements of the Declaration of Helsinki were observed, and written informed consent was obtained from the patient for all surgical procedures and publication of the clinical images.
Surgical Procedure
The patient received prophylactic antibiotics (cephalexin 1 g, Flagyl 1 g) and a corticosteroid. The procedure was carried out under general anesthesia and local anesthesia (2% carbocaine and adrenaline 1:100.000).
Because the right inferior alveolar nerve passed through the midline and was nearly exposed underneath the oral mucosa at the left lateral anterior part of the mandible, no incision was made in this anterior region. Two crestal incisions were created: the first 1 started from the position of the right lower second molar to the right lower central incisor; the second 1 started from the position of the lower left canine to the lower left first molar. A vertical release was established on each end (Fig 2). Mucoperiosteal flaps were reflected to expose the incisive branch at the lower left lateral incisor. An incision from the right central incisor to the left canine was made to connect the 2 flaps. Concurrently, reflecting the subperiosteal buccal flaps of the mental foramen and isolating the mental nerve was carefully performed. Lingual flaps were gently extended from the position of the lower right second molar to the position of the lower left first molar.
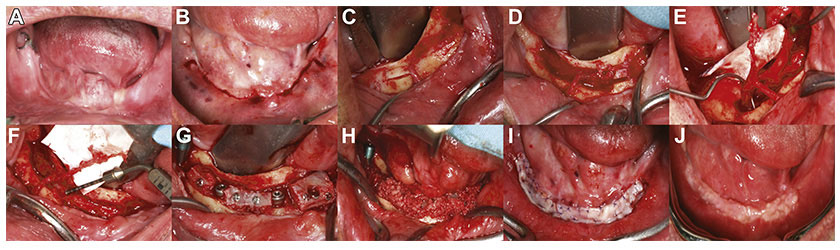
Figure 2. Intraoral images illustrating the procedure. A, A complete edentulous atrophic mandible with no keratinized tissue. B, Crestal incisions with vertical releases. C, D, Removing the cortical bone by a 5-mm segment and deflecting the inferior alveolar nerve with a protective cap attached at the end. E, Nerve branches: the inferior alveolar nerve, the mental nerve and the incisive nerve. F, The length of the right incisive branch was 22 mm. G, Implants were installed on augmented bone with miniscrews. H, Particulated iliac bone filled the bone gap. I, Soft tissue was grafted to enhance the keratinized tissue after a 2-month waiting period. J, The grafted keratinized soft tissue was healthy and stable after 2 months.
A rectangular circumference osteotomy following the outline of the right inferior alveolar nerve canal was performed using a Piezotome (Satelec, France). The osteotomy started with 5 incisions: the first 1 went upward 2 mm from the mental foramen, the second 1 went downward 2 mm from the mental foramen, the third and fourth ran parallel from the end of each first and second incision and extended 5 mm distally, and the final 1 connected the last 2 incisions to make a bone window. The cortical bone window was removed by a Freer chisel to expose the nerve. Additional 5-mm bone window segments along the IAN pathway were created to guarantee that the nerve lay in the center of the bone window. Unlike elevating long extending bone windows which were usually difficult, removing cortical bone by 5-mm segments along the IAN pathway facilitated the removal of the cortical bone, particularly in this case when cortical bone was thick. As a result, the adjacent bone was preserved, reducing the risk of bone fracture. Each step was carefully repeated to prolong the window from the mental foramen to the left lateral incisor. Furthermore, at the nerve end, we preserved a 3-mm bone segment, which was attached to the incisive branch end. This attached 3-mm piece of preserved bone served as a protective cap for clipping and dragging the nerve without touching the nerve itself. After removing the outer cortical window of the attached 3-mm piece of preserved bone, the remaining marrow bone was carefully eliminated with a curette until the inferior alveolar neurovascular bundle was exposed. The inferior alveolar nerve was retracted from the canal with a mini-periosteal elevator with gentle motion from the lower left lateral to the lower right first molar.
Autogenous bone for grafting was harvested from the iliac crest. At the donor site, a 5-cm length incision was made on the skin to the periosteum to approach the iliac crest. To avoid damaging cutaneous femoris lateralis, this first incision was 1 cm away from the spina iliac anterior superior. Subsequently, 4 incisions were made using an ultrasonic Piezotome: the first 1 was on the crest of the ilium, the second and third ones started from each end and were perpendicular to the first 1, and the final 1 connected the last 2 incisions to create a rectangular bone block. A chisel was utilized to remove the bone block with both cortical bone and cancellous bone. Hemostatic agent was placed at the donor site. The donor site was closed with sutures in 2 layers: mucoperiosteal closure and underskin closure. Bone block vertical augmentation was performed. The bone block was adjusted to fit into the recipient sites and was stabilized by 1.2-mm diameter screws.
After preparing the recipient site, endosseous Tekka (France) implants with different sizes of 4.0 × 11.5 mm, 4.0 × 10.0 mm, 4.5 × 10 mm, and 3.5 × 11.5 mm were placed on the anterior and posterior augmented regions. After inserting the fixtures, gaps between the bone graft and basal bone were filled with 2 different layers. The first layer was the particulated iliac bone, and the second layer was a mixture of autogenous particulate bone and Osteon (30% hydroxyapatite and 70% β-tricalcium phosphate). The bone window was covered by a resorbable collagen membrane (Salvin oralmem®), and the inferior alveolar nerve was allowed to lie passively under the buccal periosteum. Before closing, a horizontal releasing incision was made in the periosteum to enable a tension-free closure. After a 2-month waiting period, soft tissue graft placement and vestibuloplasty were performed to increase the zone of keratinized soft tissue around the dental implants supporting the prosthesis (Fig 2). Keratinized gingiva was harvested in the maxilla palate with a size of 40 mm × 20 mm and a thickness of 1.5 mm. It was divided into 2 pieces with a size of 40 mm × 10 mm for each and applied to the recipient.
An overdenture supported on a bar-retained, implant-supported system was delivered 6 months later (Fig 3). The prosthesis was designed with distal cantilevers, especially on the left side where the fixed prosthesis was opposed. The position of the posterior abutments on the denture was located between the premolar and molar on the right and on the mesial of the second premolar on the left (Fig 3). The left cantilever extended to 2 teeth composing the 2 molars, and the right cantilever extended to 1 tooth. On the left, the denture was adjusted so that only the mesial part of the left second molar occluded to the opposing tooth. The patient was scheduled for continuous follow-up assessments. After 3 years, the bar-retained supporting system appeared loose and was replaced with the new CAD/CAM milled bar with the OT Equator system on the same 4 implants (Fig 3). The total follow-up time was 82 months (Fig 4).
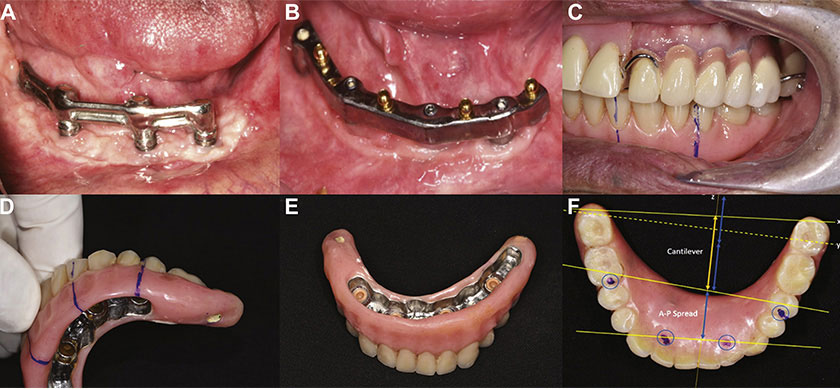
Figure 3. The secondary phase of implant placement 6 months later. A, The bar-retained supporting system and the prosthesis. B, After 3 years, the system was replaced with a new CAD/CAM milled bar-retained supporting system with the OT Equator system on the same 4 implants. C, D, E, The prosthesis with the cantilevers. F, The relation of the cantilever length (yellow arrow) and the anterior-posterior (A-P) spread (blue arrow).
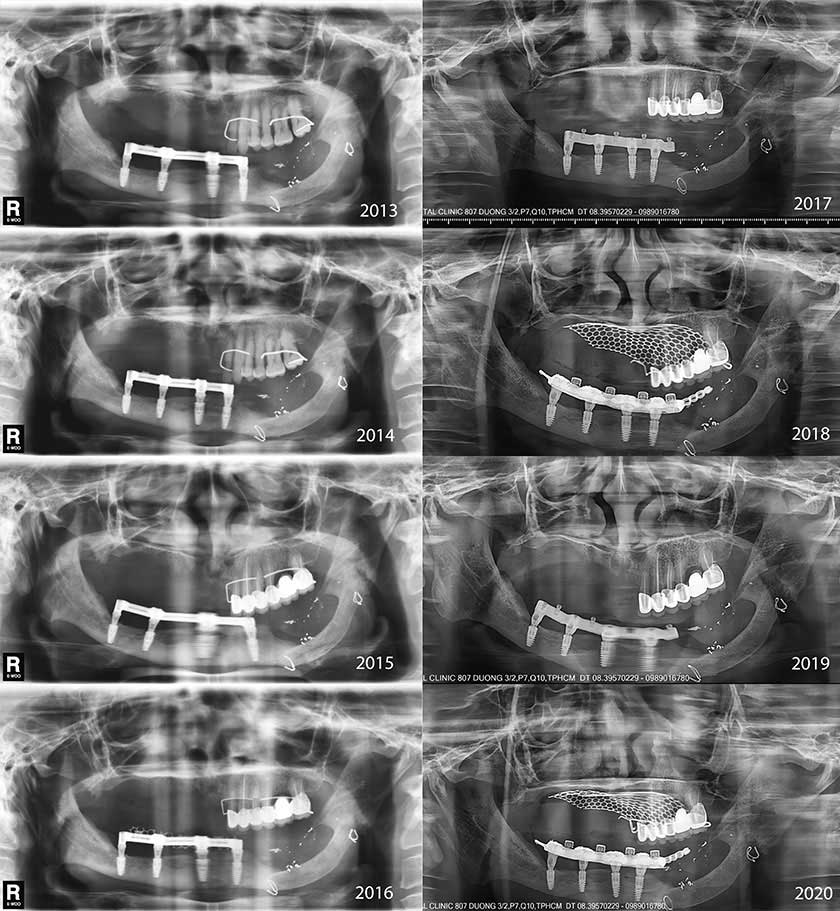
Figure 4. Orthopantomographic images of annual follow-ups from 2013 to 2020 present peri-implant health with good osseointegration.
Postoperative Care
The patient was discharged 24 hours after surgery. Postoperative measures consisted of antibiotic administration for 7 days (Augmentin 2 g/day, Flagyl 1.5 g/day), analgesics for 5 days, and 0.12% chlorhexidine mouthwash for 14 days.
Actual Outcome
The 4 installed implants presented good initial stability (35 N/cm) and good osseointegration based on an orthopantomographic image (Fig 3). Bone remodeling was observed around the implant shoulder. The zone of keratinized soft tissue around the dental implants and supporting overdenture was expanded.
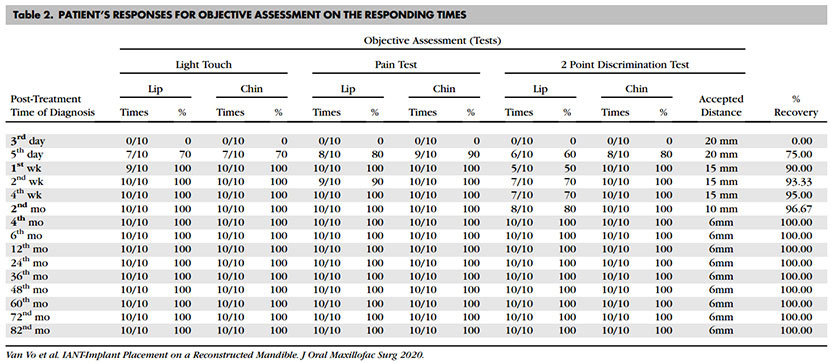
To evaluate neurofunctional recovery, a range of tests were performed to assess the subjective and objective responses of the patient.13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26 For the subjective evaluation, the patient completed a questionnaire (Fig 5). The patient was instructed to identify sensory factors, including hypothesia, tickling, burning, pain, pinching, numbness, and anesthesia. Based on the questionnaire results, although the patient reported numbness and pain at the beginning, he overall presented satisfaction regarding to the function, esthetic, and significantly improved the quality of life (Table 1). For the objective assessment, the nociceptive receptors were evaluated with 2 different tests: a light touch test and a pain test.13,16 The patient was able to choose 1 type of feeling, such as dull ache, pain, or sharp. The sensitivity was judged good if the patient responded sufficiently with increasing stimulation. The light touch test showed that the patient did not respond during the first 3 days. After 1 week, the patient was able to respond 9 of 10 times on the lips and chin areas. The patient fully recovered the light touch sensory after 2 months. In addition, the pain test was conducted with a large needle (30 gauge). The patient also showed no response during the first 3 days and fully recovered after only 1 week on both lips and chin areas. The mechanoreceptor was evaluated with a 2-point discrimination test15 using a compass with 2 blunt metal tips. The 2 tips were applied with the same pressure, and the distance between the tips was reduced until the patient could no longer correctly discriminate the 2 points. A 6 mm distance was a minimal gap to be considered an adequate response.17 For the first 3 days, the patient could not distinguish the 2 points with 20-mm-distance points. After the first week, he could respond 5 of 10 times to 15-mm-distance points. Two months later, he could react sufficiently at a distance of 10 mm, and after 4 months, his response was completely correct at a distance of 6 mm. Ultimately, based on the objective assessment results, the sensory recovery significantly increased by 90% after 1 week, recovered by 97% after 2 months and totally recovered after 4 months (Table 2).
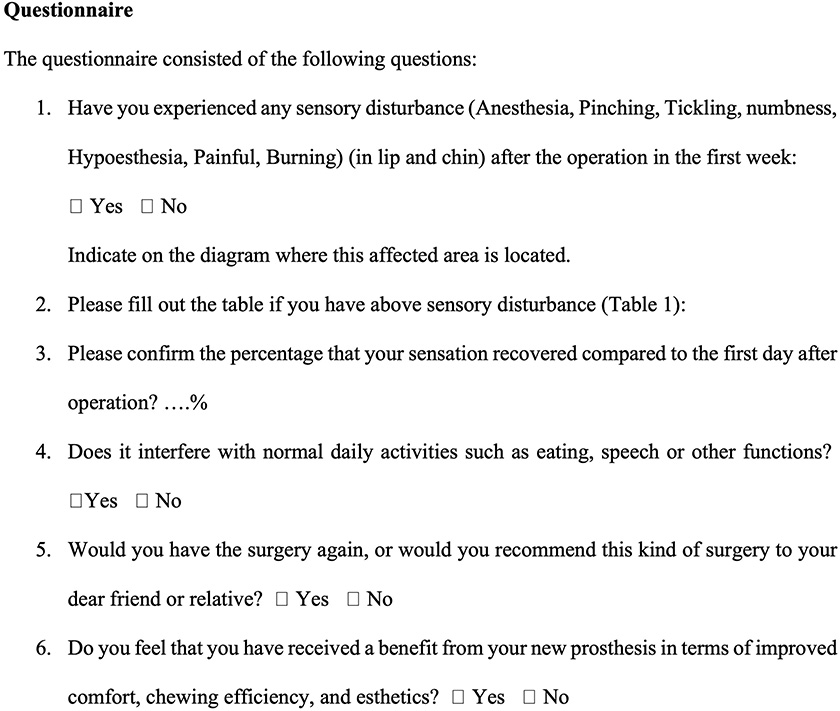
Figure 5. A questionnaire was administered to patients for subjective assessment of outcome.18, 19, 20
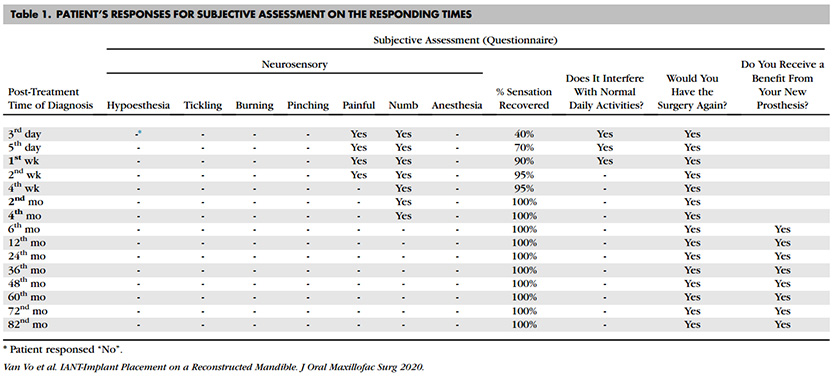
After 7 years, all 4 dental implants remained stable and functioned well without any problems. The IBG maintained good quality based on orthopantomography. The peri-implant and soft tissues were healthy. The patient was satisfied with the esthetic and functional outcomes of the prosthesis. No nerve dysfunction was reported.
Discussion
In recent years, IANT has been widely used as an alternative to short implants or bone grafts for implant-based treatment for the atrophic edentulous jaw, which does not have sufficient bone volume for a conventional approach. In this case, the alveolar ridge lacked the required minimum height (8 mm) for implant placement,9 and the passage of the right inferior alveolar nerve crossed the mandibular midline; thus, simultaneous IANT and IBG were indicated to create a sufficient bone volume to support the implants. Another disadvantage in this case was the previously reconstructed bone on the left side which were deviated from the mandibular arch. In fact, it was nearly impossible to place the implant on this rebuilt area. Consequently, the most distal area that allowed the implant to be installed was on the mesial part of the lower left second molar.
IANT has some postoperative complications, including some degree of sensory alterations.6 Nerve dysfunction in the lips occurs in all patients to various degrees and for various durations ranging from 1 to 6 months.22,23 These complications result from a certain degree of traction and/or pressure on the neurovascular bundle during surgery.24 The recovery time may be reduced depending on the type of osteotomy devices used. A higher rate of complications was reported with rotary burs than with a Piezotome. In 2001, Hori et al.25 reported that 5 of 6 (83%) patients who underwent IANT with implant placement still suffered from neurosensory disturbances after 3 years. From 1996 to 2002, Ferrigno et al.26 performed 19 IANT procedures on 15 patients, 1 of whom (6.6%) reported that the change in sensation was persistent after 6 1/2 years. Moreover, in 2013, Diaz and Gias 27 published a study on 15 patients, with 47.4% completely recovering after the first week and 94.7% having normal neural function after 2 months. According to Metzger et al.,23 osteotomy surgery with a piezoelectric device provides a more straightforward and safer approach in terms of protecting the inferior alveolar nerve from injury than osteotomy surgery with rotary instruments. In this case, a piezoelectric device was utilized to achieve a more predictable outcome. In addition, the creation of a 3-mm bone cap attached to the end of the left incisive branch was used as a point for clipping and repositioning the incisive nerve without damaging the nerve. This technique creates 1 free end that can eliminate the stretching force, reduce the physical force to the nerve, and decrease the risk of neural injury, which helps to recover neural dysfunction in a short amount of time. With minimal physical intervention, the patient reported that the sensory dysfunction resolved in a short amount of time. After experiencing lip numbness in the first 5 days postoperatively, the sensory was recovered significantly by 90% 1 week later to 97% after 2 months. In 2002, Morrison reported an initial decrease in sensation lasting approximately 1 month.24 According to Rosenquist,9 77% of patients had resolved sensation dysfunction after 6 months, which is a shorter recovery period than those in other similar studies.
With regard to sensory dysfunction, IANT was conducted in this study because of the special pathway of the right mandibular canal. According to Mraiwa et al.,18 only 18% of the incisive branches of inferior alveolar nerves terminate at the midline, whereas most end at the lateral or central incisor apex. In this case, the right incisive branch crossed to the contralateral region. If the right inferior alveolar nerve was not transposed, the placed implant would have encroached on the incisive branch of the inferior alveolar nerve, resulting in neural dysfunction. In a case report by Kohavi and Bar-Ziv 19 in 1996, a 68-year-old patient suffered from sensory discomfort after an implant placement procedure in the anterior mandibular as the incisive nerve extended to the midline. Consequently, IANT was the only optimal option in this specific case. The incisive branches of inferior alveolar nerves rarely terminate at the contralateral side, while most end at the ipsilateral or central incisor apex. The right incisive nerve extended across the midline, possibly to intervene for the reconstructed region, which had no neurointervention after the surgery 40 years previously. In this case, the right incisive branch crossed to the contralateral region. The length of the incisive branch in this case was 22 mm, longer than the mean length of the normal incisive canal, which is 9.8 ± 3.8 mm.28
The disadvantages of a short implant in an advanced resorption ridge are poor initial stability and an inappropriate implant-crown ratio. IANT has long been used and has demonstrated to be efficient for implant placement procedures in which using longer implants resulted in a better proportion between the implant and prosthesis.13,20 Using suitably sized implants will also help maintain the proper implant-crown ratio for prosthetic rehabilitation in the future. IANT enabled the 4 implants to be anchored in cortical bone and achieved good initial stability. In addition, the IANT technique allows implants to be placed in the right dimension and minimizes biomechanical nonaxial stress.21
In terms of bone reconstruction, IBG overcomes bone graft regeneration in both the vertical and horizontal dimensions.11,29 In this study, the harvested IBG was a bone block consisting of bone marrow and cortical bone. The bone marrow contains many osteoblasts and growth factors that lead to enhanced bone healing.30,31 Although the bone marrow was placed inward to stimulate healing, the cortical bone was turned outward to utilize biomechanical rigidity and to limit bone resorption. Implants were splinted by a bar to prevent overloading during function. The bone healed well, and implant osteointegration was observed after 4 1/2 months. However, the remodeled bone around the implant must be followed for 6 to 12 months.22 Thus, the patient was scheduled for continuous follow-up assessments for the next 7 years and presented a very satisfactory result, including well-osteointegrated implants and healthy augmented bone.
Free soft tissue grafting on the whole lower arch is a complicated procedure due to limitations of the donor site. Apart from the risk of bleeding, many important structures are situated on the palate, such as the greater and lesser palatal neurovascular bundles, precluding harvesting of a large amount of tissue at one time. To prevent possible complications, a customized stent was placed immediately after harvest for hemostasis. In addition, the stent helped to keep the graft in place during masticatory function. Consequently, during 7 years of monitoring, the implants were surrounded by the increased zone of keratinized tissue without inflammation or recession. Grafting keratinized tissue provided a wider keratinized tissue zone and ensured long-term success of the dental implant.32
The overdenture was designed to maintain long-term esthetic and functional use. For the overdenture on 4 implants, the amount of distal cantilever is closely related to the anterior-posterior (A-P) spread of the denture.33 Superimposing the locations of the 4 abutments on the occlusal surface of the denture helped to locate the landmarks that were used to value the relation of cantilever length (yellow line) and the A-P spread (blue line) (Fig 3E). The line of posterior-most cantilever (the distal most of the second molars) was the x line. According to Carl Misch,33 the cantilever length to the x line (Fig 3E) was 1.5 times the A-P spread. In this case, only the mesial half of the left second molar contacted the opposing tooth, which reduced the loading stress; therefore, the cantilever length measured from the occlusal contact points of both sides (y line) was just 1.25 times the A-P spread. This length is suitable to the Misch recommendation for cantilever. As a result, all 4 implants maintained good osseous integration and minimized bone loss during the 7-year follow-up, presenting orthopantomographic evidence.
Performing IANT and IBG simultaneously is not a common operation. The procedure is technically sensitive and requires experienced surgeons, strict selection criteria for patients, and proper instruments. In cases where the bone height and volume are insufficient for implants, the surgeon has no other option except for IANT.
In conclusion, despite scientific and medical advances, an immediate implant placement procedure after a complex surgery involving mandibular reconstruction and iliac bone grafting remains challenging. Particularly, if a patient has already undergone large basal bone reconstruction, a standardized treatment approach is not possible. If the remaining bone is insufficient, IANT may represent the only treatment option. Properly isolating the nerve and using a piezotome will help the surgeon prevent nerve injury and help the patient recover in a short amount of time. One-stage implant placement can provide a satisfactory result and minimize the amount of surgery. Indeed, the patient was followed for 7 years and had good osseointegration around the implants and an iliac bone graft with good quality. The patient was satisfied with the esthetic and functional outcomes of the prosthesis.
Acknowledgments
The authors would like to thank Dr. Le Duc Lanh, Dr. Vo Chi Hung, Dr. Ta Anh Tuan, and Dr. Nguyen Tai Son, for their assistance in this case report.
References
- Y. Mittal, G. Jindal, S. Garg: Bone manipulation procedures in dental implants. Indian J Dent, 7 (2016), p. 86
- P. Proussaefs: Vertical alveolar ridge augmentation prior to inferior alveolar nerve repositioning: A patient report. Int J Oral Maxillofac Implants, 20 (2005), p. 296
- W.C. Polo, P.R. Cury, W.R. Sendyk, A. Gromatzky: Posterior mandibular alveolar distraction osteogenesis utilizing an extraosseous distractor: A prospective study. J Periodontol, 76 (2005), p. 1463
- I.A. Urban, A. Monje: Guided bone regeneration in alveolar bone reconstruction. Oral Maxillofac Surg Clin North Am, 31 (2019), p. 331
- N. Jain, M. Gulati, M. Garg, C. Pathak: Short implants: New horizon in implant dentistry. J Clin Diagn Res, 10 (2016), p. Ze14
- B. Abayev, G. Juodzbalys: Inferior alveolar nerve lateralization and transposition for dental implant placement. Part I: A systematic review of surgical techniques. J Oral Maxillofac Res, 6 (2015), p. e2
- C.C. Alling: Lateral repositioning of inferior alveolar neurovascular bundle. J Oral Surg, 35 (1977), p. 419
- O. Jensen, D. Nock: Inferior alveolar nerve repositioning in conjunction with placement of osseointegrated implants: A case report. Oral Surg Oral Med Oral Pathol, 63 (1987), p. 263
- B. Rosenquist: Implant placement in combination with nerve transpositioning: Experiences with the first 100 cases. Int J Oral Maxillofac Implants, 9 (1994), p. 522
- D. Buser, K. Dula, U. Belser, et al: Localized ridge augmentation using guided bone regeneration. 1. Surgical procedure in the maxilla. Int J Periodontics Restorative Dent, 13 (29) (1993)
- T.T.H. Nguyen, M.Y. Eo, T.S. Kuk, et al. Rehabilitation of atrophic jaw using iliac onlay bone graft combined with dental implants. Int J Implant Dent, 5 (2019), p. 11
- J.I. Cawood, R.A. Howell: A classification of the edentulous jaws. Int J Oral Maxillofac Surg, 17 (1988), p. 232
- H.M. Hashemi: Neurosensory function following mandibular nerve lateralization for placement of implants. Int J Oral Maxillofac Surg, 39 (2010), p. 452
- A. Morrison, M. Chiarot, S. Kirby: Mental nerve function after inferior alveolar nerve transposition for placement of dental implants. J Can Dent Assoc, 68 (2002), p. 46
- S. Al-Almaie, A.M. Kavarodi, A. Al Faidhi, et al. Incidence of neurosensory disturbance and success rates of solid-screw implants placed in conjunction with inferior alveolar nerve transposition. Ann Maxillofac Surg, 10 (2020), p. 80
- C.E. Misch, R. Resnik: Mandibular nerve neurosensory impairment after dental implant surgery: Management and protocol. Implant Dent, 19 (2010), p. 378
- G. Gasparini, R. Boniello, G. Saponaro, et al. Long term follow-up in inferior alveolar nerve transposition: Our experience. Biomed Res Int, 170602 (2014), p. 2014
- N. Mraiwa, R. Jacobs, P. Moerman, et al. Presence and course of the incisive canal in the human mandibular interforaminal region: Two-dimensional imaging versus anatomical observations. Surg Radiol Anat, 25 (2003), p. 416
- D. Kohavi, J. Bar-Ziv: Atypical incisive nerve: Clinical report. Implant Dent, 5 (1996), p. 281
- A. Sethi, S. Banerji, T. Kaus: Inferior alveolar neurovascular bundle repositioning: A retrospective analysis. Int J Oral Maxillofac Surg, 46 (2017), p. 518
- B. Rosenquist: Fixture placement posterior to the mental foramen with transpositioning of the inferior alveolar nerve. Int J Oral Maxillofac Implants, 7 (1992), p. 45
- A. Lorean, F. Kablan, Z. Mazor, et al. Inferior alveolar nerve transposition and reposition for dental implant placement in edentulous or partially edentulous mandibles: A multicenter retrospective study. Int J Oral Maxillofac Surg, 42 (2013), p. 656
- M.C. Metzger, K.H. Bormann, R. Schoen, et al. Inferior alveolar nerve transposition: An in vitro comparison between piezosurgery and conventional bur use. J Oral Implantol, 32 (2006), p. 19
- A. Hassani, M.H.K. Motamedi, S. Saadat: Inferior alveolar nerve transpositioning for implant placement. Oral Maxillofac Surg, 26 (2013), pp. 659-693
- M. Hori, T. Sato, K. Kaneko, et al. Neurosensory function and implant survival rate following implant placement with nerve transpositioning: A case study. J Oral Sci, 43 (2001), p. 139
- N. Ferrigno, M. Laureti, S. FanaliInferior alveolar nerve transposition in conjunction with implant placement. Int J Oral Maxillofac Implants, 20 (2005), p. 610
- J. Fernández Díaz, L. Naval GíasRehabilitation of edentulous posterior atrophic mandible: Inferior alveolar nerve lateralization by piezotome and immediate implant placement. Int J Oral Maxillofac Surg, 42 (2013), p. 521
- P. Pereira-Maciel, E. Tavares-de-Sousa, M.A. Oliveira-SalesThe mandibular incisive canal and its anatomical relationships: A cone beam computed tomography study. Med Oral Patol Oral Cir Bucal, 20 (2015), p. e723
- A. Sethi, T. Kaus, J.I. Cawood, et al.Onlay bone grafts from iliac crest: A retrospective analysis. Int J Oral Maxillofac Surg, 49 (2020), p. 264
- M.N. Knight, K.D. Hankenson: Mesenchymal stem cells in bone regeneration. Adv Wound Care (New Rochelle), 2 (2013), p. 306
- P. Felice, R. Pistilli, G. Lizio, et al. Inlay versus onlay iliac bone grafting in atrophic posterior mandible: A prospective controlled clinical trial for the comparison of two techniques. Clin Implant Dent Relat Res, 11 (Suppl 1) (2009), p. e69
- S.J. Narayan, P.K. Singh, S. Mohammed, R.K. Patel: Enhancing the zone of keratinized tissue around implants. J Indian Prosthodont Soc, 15 (2015), p. 183
- C.E. Misch: Mandibular and maxillary implant overdenture design and fabrication. C.E. Misch (Ed.), Dental implant prosthetics, Elsevier, St. Louis, Missouri (2015), pp. 753-828